Have you ever experienced a sharp, nagging back pain that just won’t go away? There can be several causes of this pain, but one of the most common causes is a herniated disc. You may ask what is a herniated disc. It is a condition in which the discs between your backbone (vertebra) slip or rupture. It often leads to discomfort, tingling, and even weakness in the muscles.
So, what exactly causes a disc to herniate? And more importantly, how do you treat it? To understand the most common causes of disc herniation, recognize early symptoms, and know the most recommended treatment for disc herniation, read further and dive into the details.
What is a Herniated Disc?
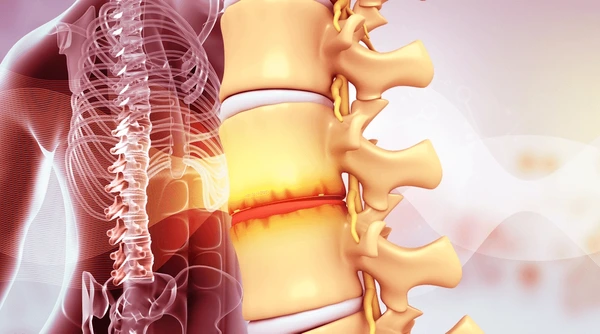
Let us first get a little idea about your spine to understand more about a herniated disc. You can think of your spine as a stack of bones, and between each bone, there is a soft, jelly-like disc. These discs cushion your vertebrae to absorb any shock. As a result, your spine remains flexible and strong.
But what happens when one of these discs slips out of place or ruptures? Well, that’s a herniated disc! The disc itself has an outer covering, and when this covering tears, it lets the inner gel push out. This leaked gel can irritate the nerves nearby. In turn, this causes pain, numbness, or weakness. Sounds uncomfortable, right? Now, let’s explore the most common causes of disc herniation.
What Are The Most Common Causes of a Herniated Disc?
So, what exactly causes a disc to herniate? Let’s break it down-
Age-related Degeneration:
The most common cause of disc herniation is age-related degeneration. As you get older, your spinal discs start to lose water content. It makes them less flexible and, hence, more prone to tearing or rupturing.
Sudden Injury or Trauma:
Age isn’t the only culprit for a herniated disc. Sudden trauma or injuries can also cause a disc to herniate. Have you ever lifted something heavy the wrong way or experienced a fall? These sudden movements can cause a disc to push out of its normal space. As a result, you may start experiencing pain and discomfort.
Repetitive Motion or Strain
Repetitive motions and strain are other big contributors. Poor posture, sitting for long periods, or repeated heavy lifting can cause slow wear down of your discs over time. In such cases, even a small movement can trigger a herniation after years of strain.
Genetic Predisposition
Genetics can also play a significant role in herniation. If disc problems run in your family, then you are more likely to suffer from herniation. So, some people are simply more predisposed to developing disc issues no matter how careful they are.
Now that you already know the major causes of disc herniation, how will you identify whether you suffer from it? To identify disc herniation, you must first recognize its symptoms.
What Are The Symptoms of a Herniated Disc?
You can suffer from various symptoms depending on where the disc is located and how severely it presses the nerve close by. Here are some of the most common signs-
Back or neck pain
One of the first indicators is constant back or neck pain. If the herniated disc is in your lower back, you will feel the pain there. Likely, if it is in your neck, you’ll feel discomfort in that region.
Numbness or Tingling in Limbs
Do you experience a “pins and needles” sensation? Well, a herniated disc often tends to cause this feeling. It is especially felt in your arms, legs, or other areas because the disc puts pressure on the nerves.
Weakness in Muscles
Has it become harder to lift objects or move around? Muscle weakness is another symptom of disc herniation. This weakness happens when your disc is compressing a nerve, which makes everyday tasks more difficult for you.
Sciatica (for Lumbar Herniation)
It is a condition in which you feel sharp, shooting pain from your lower back down one leg. It is a direct indication of a herniated disc in the lumbar region of your back.
Do not panic if you suffer from these symptoms, as several treatment options can cure your herniated disc.
How to Treat Herniated Discs?
Now let’s answer the questions that you may have about the treatment of herniated discs, like what is the fastest way to heal a herniated disc or what is the most recommended treatment for disc herniation.
See, a herniated disc has multiple possible treatments, and it depends on the severity of your condition and which treatment the doctor suggests. Here are some of the most common treatments for disc herniation.
Pain Relief Medication and Physical Therapy
Many people are unaware of the fact that a herniated disc can heal on its own. Yes, a herniated disc mostly heals on its own, and what you are left to treat is the pain during the healing period. So, you can simply use over-the-counter pain relief medication to help you manage the pain.
Moreover, you can make the process of healing faster with the help of physical therapy. With physical therapy, the compression of the disc and pressure can be released, which not only decreases the pain but also helps to make the healing process faster. But what if the pain doesn’t completely vanish for a longer time?
Endoscopic Disc Decompression and Regenerative Treatment
If the pain doesn’t fade away for a longer period of time, average between 6 to 8 weeks, then the most recommended treatment for disc herniation is minimally invasive endoscopic disc decompression. This method is one of the best treatments for more severe cases because it doesn’t need bigger incisions and tissue disruption during the procedure.
Let’s say you have an L5 S1 disc herniation, and then how do you treat the L5 S1 disc herniation? The doctor will use regional anesthesia first to ensure you feel no pain. Then, a small incision will be made, and the procedure will be performed through an endoscope that has a camera to visualize it. After that, the recovery process will take place.
Here, if you opt for regenerative treatment combined with the endoscopic process, recovery will be faster. The doctor will implant ortho biologics derived from your own blood or bone marrow concentrate. With this treatment, the recovery will be significantly faster, and in a lot of cases, only regenerative orthobiologics implantation into the functional spine unit’s most painful areas is enough to help you recover from your pain.
Traditional Surgery
While it’s rare that traditional surgery is needed, you must be aware of this treatment as well. Almost 90% of the total cases get cured with the above methods, and the need for surgery arises in emergency cases. Sometimes, the nerve gets seriously affected, which can even lead to problems like loss of bowel and bladder control, which is known as Cauda equina syndrome.
The surgery is mainly invasive; thus, it increases the recovery time compared to other methods. However, if you start physical therapy on time, you’ll be able to significantly decrease the recovery time. Additionally, there are some other factors that constitute the recovery, like the patient’s age, health, etc.
Wrapping Up
In conclusion, understanding herniated discs is crucial for identifying early symptoms like pain, numbness, or weakness. With various treatment options such as medication, physical therapy, and minimally invasive procedures, most cases can be effectively managed. Early diagnosis and appropriate treatment help ensure faster recovery and prevent complications.
Frequently Asked Questions
There can be various reasons why herniated discs can occur but yes there are some causes that lead to most herniated disc cases. One such cause is living heavy weight in an improper form leading to excess pressure on the disc. This excess pressure can tear the outer covering of the cushion-like material in the disc and it bulges out. This bulged material compresses the nerves going through the spine which is what mainly causes the discomfort and pain.
Since herniated disc can heal on its own, the primary treatment options can be conservative. For instance, pain relief medication to deal with pain, methods like RICE and physiotherapy to deal with inflammation, and help in recovery. However, if the case is more severe with less chance of healing on its own, minimally invasive surgical intervention can be done to get rid of the herniated disc and its symptoms.
Back pain is the main sign of herniated disc but it can occur due to other conditions as well. So, if there’s a radiating pain from the lower body to the leg and weakness, tingling, and numbness in the limb, then it can be a case of a herniated disc. It occurs because a herniated disc can cause irritation to the nerves passing through the spine.
While it’s rare to have an emergency case of a herniated disc, a condition called Cauda Equina Syndrome may show its symptoms and it must be gotten rid of as soon as possible. In this case, the patient loses control over the muscles of the limb and also loses the ability to urinate and pass stool by himself. The only treatment for this condition is a surgical intervention which should be done immediately.
Getting symptoms of worsening of a bulging disc is not possible as there are no dedicated symptoms. If the pain and discomfort are increasing as per the patient or the location of the pain is getting bigger, then it may reflect the worsening of the situation. However, the clear symptoms of a worse herniated disc case are the inability to urinate or pass stool which are the symptoms of Cauda Equina Syndrome.
At Axis, we have a range of treatments for herniated but we always choose a method based on the diagnosis. Moreover, we always aim to fix the patient’s problem without surgery, that’s why we always opt for a conservative approach which allows us to treat the condition without disturbing the natural integrity of the spine. However, in some cases, minimally invasive surgery may be required. In such a case we do a targeted endoscopic disc decompression under local anesthesia which makes the treatment painless.